Medicaid Unit 510-05-35-05
(Revised 10/1/13 ML #3390)
View Archives
(N.D.A.C. Section 75-02-02.1-08)
For Applications and Reviews Received on or After October 1, 2013 for benefits beginning January 1, 2014:
- MAGI Methodologies
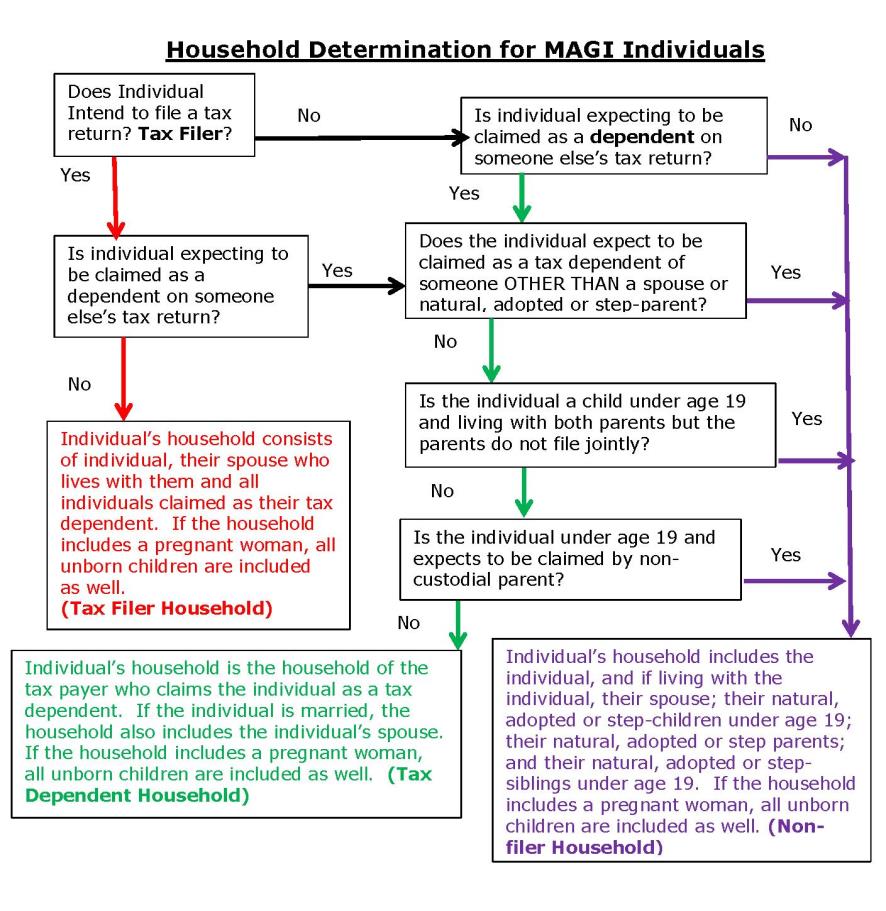
Each individual will have his/her own Medicaid household determined as follows—in the following order:
- Does this individual expect to file taxes?
- If “No”, continue to step b below.
- If “Yes” – Does the individual expect to be claimed as a tax dependent by someone else?
A. If “Yes” – Continue to step b below.
B. If “No” – The individual’s Medicaid household consists of the taxpayer, the spouse living with the taxpayer, and all persons whom the taxpayer expects to claim as a tax dependent. This is known as the tax filer household.
- Does the individual expect to be claimed as a tax dependent?
- If “No” – Continue to step c below.
- If “Yes” – Does the individual meet any of the following exceptions?
- The individual expects to be claimed as a tax dependent of someone other than a spouse, or natural, adopted or step parent.
- The individual is a child under age 19 and is living with both parents but the parents do not file a joint tax return.
- The individual is a child under age 19 and expects to be claimed by a non-custodial parent.
A. If “Yes” – continue to step c.
B. If “No” – the household is the household of the taxpayer that claims the individual as a tax dependent. If the individual is married, the household also includes the individual’s spouse. This is known as the tax dependent household.
- For individuals who neither expect to file a tax return nor expect to be claimed as a tax dependent, or who meet one of the exceptions under 1(b)(ii), the household consists of the individual, and if living with the individual—
- The individual’s spouse
- The individual’s natural, adopted or step children under age 19; and
- The individual’s natural, adopted or step parents, and natural, adopted or step siblings under age 19. This is known as the non-filer household.
The following flow chart illustrates this:
NOTE: Under MAGI Methodologies, individuals may no longer be opted out of a household.
- Non-MAGI Methodologies:
When a child is included in the Medicaid unit eligibility is pursued for the child unless:
- The child is eligible under the Healthy Steps Program;
- The child is an ineligible alien or the child's US citizenship or identity has not been verified after allowing a reasonable opportunity to provide the verifications;
- The child’s Social Security Number (SSN) has not been provided; or
- The child is receiving services in a Psychiatric Residential Treatment Facility (PRTF), or the state hospital, the Prairie at St. John's center, the Stadter Psychiatric Center, or any other institution for mental disease (IMD), and has not obtained certification of need for services in that facility.
When a caretaker chooses not to include a child in the Medicaid unit, the child is not included in the unit for any other purpose. This applies to non-MAGI households only.
Non-MAGI Medicaid Households and for Applications and Reviews received Prior to January 1, 2014 for benefits required prior to January 1, 2014 for children and families:
- A Medicaid unit may be one individual, a married couple, or a family with children under twenty-one years of age, or if blind or disabled under age eighteen, whose income and assets are considered in determining eligibility for any member of that unit, without regard to whether the members of the unit all physically reside in the same location.
A single 18 year old disabled individual is included in the parental Medicaid unit if choosing to be treated as a child, or in a separate case and not included in the parental Medicaid unit if choosing to be eligible as a disabled individual.
- An applicant or recipient who is also a caretaker of children under twenty-one years of age may select the children who will be included in the Medicaid unit. Anyone whose needs are included in the unit for any month is subject to all Medicaid requirements which may affect the unit. The financial responsibility of relatives must be considered with respect to all members of the assistance unit.
When a child is included in the Medicaid unit eligibility is pursued for the child unless:
- The child is eligible under the Healthy Steps Program;
- The child is an ineligible alien or the child's US citizenship has not been verified;
- The child is ineligible due to no medical need (client share (recipient liability) exceeds need);
- The child is receiving services in a Psychiatric Residential Treatment Facility (PRTF), or the state hospital, the Prairie at St. John's center, the Stadter Psychiatric Center, or any other institution for mental disease (IMD), and has not obtained certification of need for services in that facility; or
- The child's identity has not been verified.
When a caretaker chooses not to include a child in the Medicaid unit, the child is not included in the unit for any other purpose (e.g. in the budget, in the asset test, or to create eligibility for a caretaker).

